Correct Coding Initiative
Background
The National Correct Coding Initiative (NCCI) function identifies CPT code combinations (occurring on the same patient for the same DOS) based upon published NCCI edits that may require modifiers to bypass payer edits. Additionally, when 2 or more of the same CPT codes occur on the same patient for the same DOS (hereinafter referred to as recurrent CPT codes), these coding scenarios may also require the addition of modifiers. Bilateral procedures can be billed twice per day and may require a different set of modifiers and verification against the ICD-10 code. Multiple procedure payment reduction (MPPR) edits necessitate the addition of a modifier 59 or X modifier to avoid MPPR payment reductions.
All this presumes the Client has appropriate processes in place to ensure the accuracy of the CPT coding prior to appending modifiers. Also, while there are thousands of NCCI edits in published material, not all edits apply to radiology, not all edits require modifiers, some edits may require manual review prior to adding the modifier(s) and not all payers edit on ALL NCCI combinations.
Covalent employees will maintain the tables for the editing required under these processes. The tables will use place of service (POS), insurance code and/or class, column 1 CPT code (C1), column 2 CPT code (C2), an indicator to either automatically add the modifier or send the charge to manual review and modifier designation. If a field is blank, then all charges are tested unless a table specifically exists for that POS or insurance code and/or class. The utilization of insurance code and class must allow for and/or testing statements, for example, “insurance class is EQ to 55 and insurance code is NE to 4300”. The bilateral table will also have ICD-10 designations that are appropriate for use with any of the bilateral modifiers (LT, RT, T1, T6 etc.).
The logic of utilization of the tables must first test POS, then insurance code and/or class, then CPT etc. Insurance code and/or class must be second to allow for designating a different modifier (say and X modifier for 1 payer and a 59 for another payer) for the same CPT code combinations.
Process Flows:
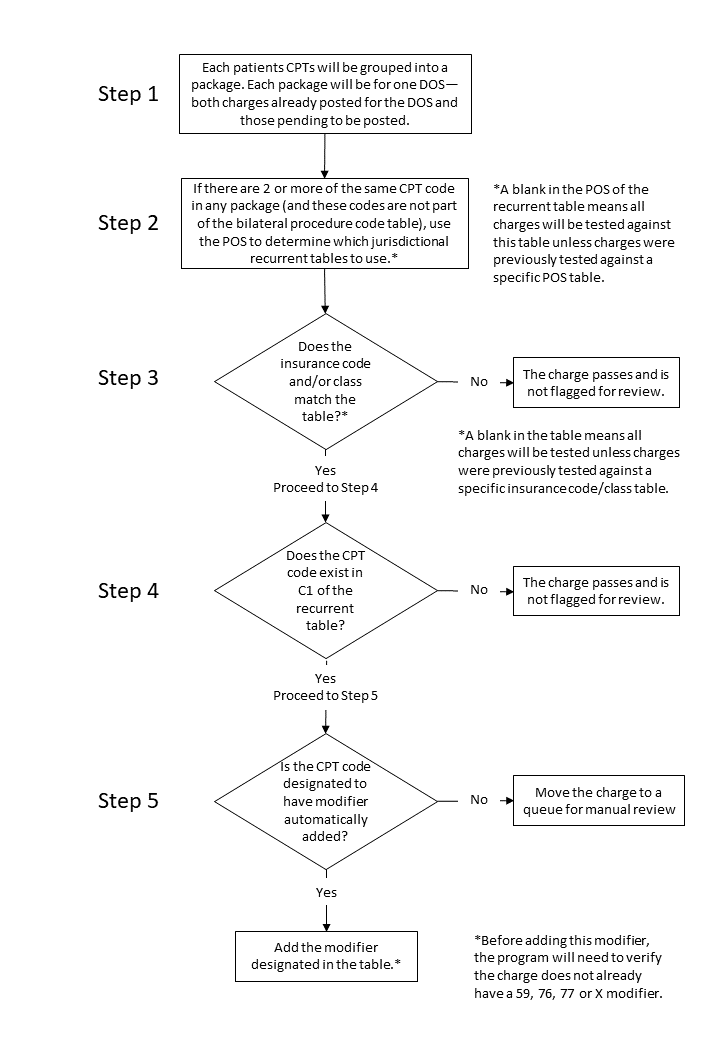
1. Recurrent CPT Codes
MI will use the following process flow to determine correct modifiers to either automatically add to the charge or send the charge to a queue for further review. A recurrent table will be maintained. This table will have no value in C2 and only values in C1 will be used for testing.
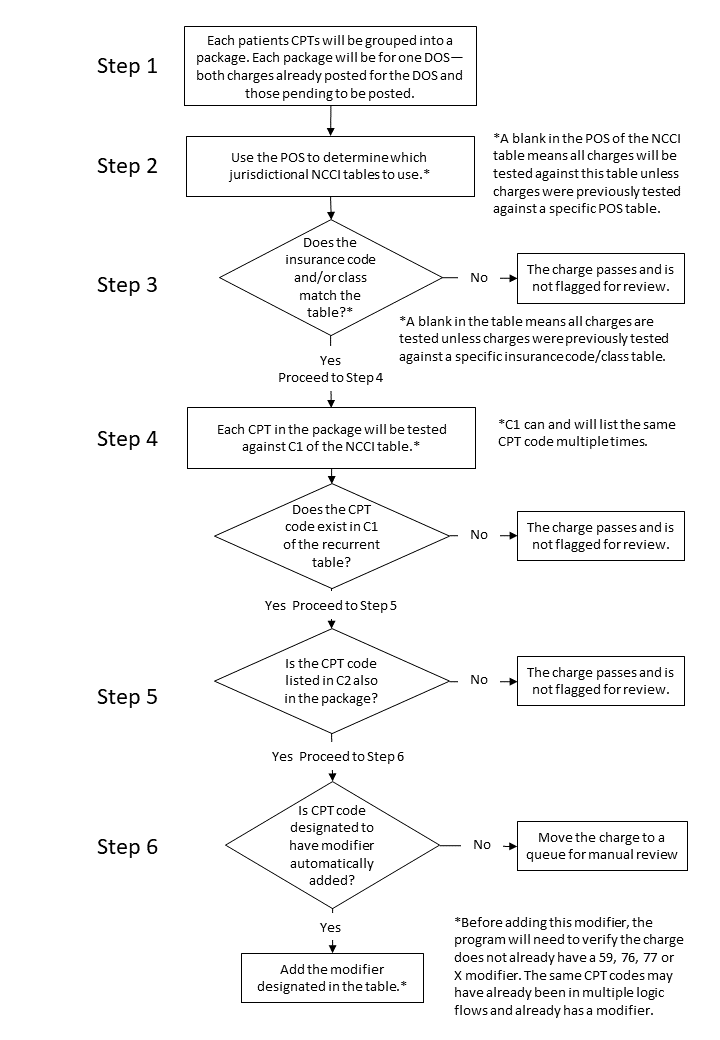
2. NCCI Edits CPT Codes
MI will use the following process flow to use the tables to determine correct modifiers due to NCCI edits.
3. Bilateral Edits CPT Codes
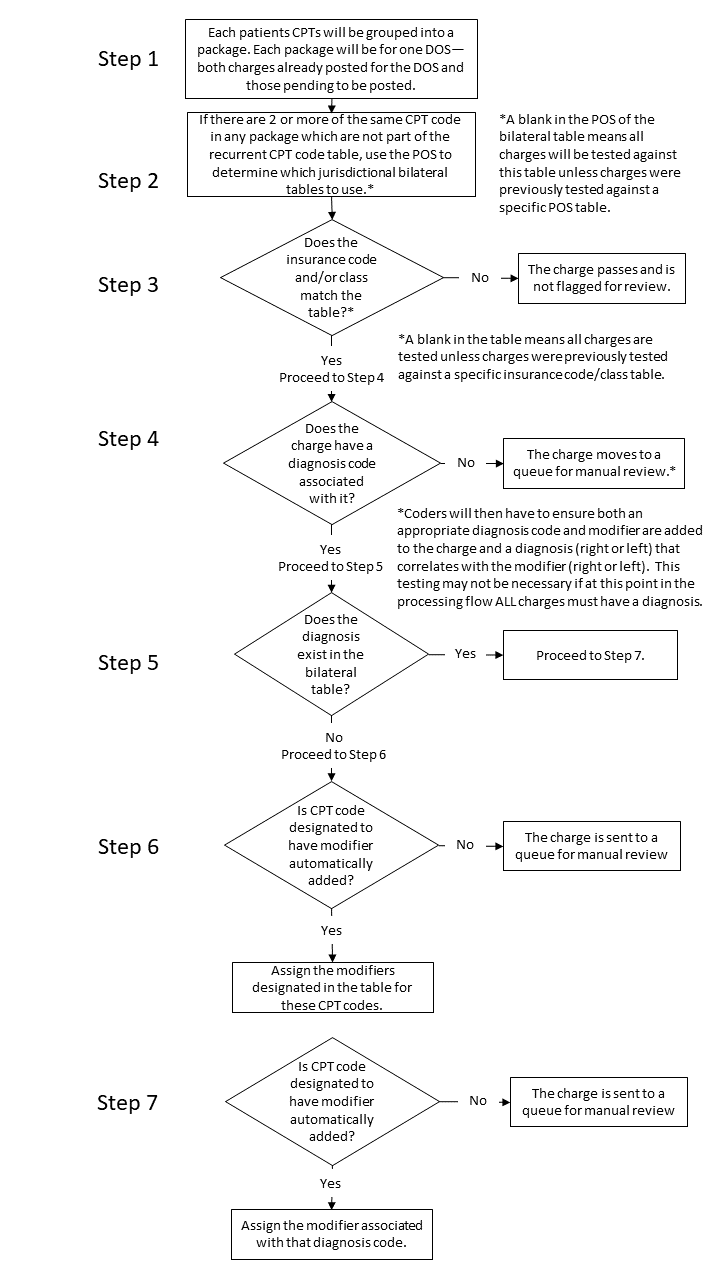
The bilateral tables will be built as follows:
- Assume a complete foot on both the left and right (CPT code 73630)
- Assume fracture. S92.001 is right calcaneus and S92.002 is left calcaneus.
- 73630 will be built with S92.001 and RT (along with all other diagnosis codes with a right designation).
- 73630 will also be built with S92.002 and LT (along with all other diagnosis codes with a left designation).
- In step 6 above, the program will simply assign an RT and an LT, one to each CPT code, without regard to the diagnosis code.
- In Step 7 above, the program will assign an RT if the diagnosis code is built in the table with the RT mmodifier or an LT if the diagnosis code is built with the LT modifier and if neither, the change goes to a queue for review.
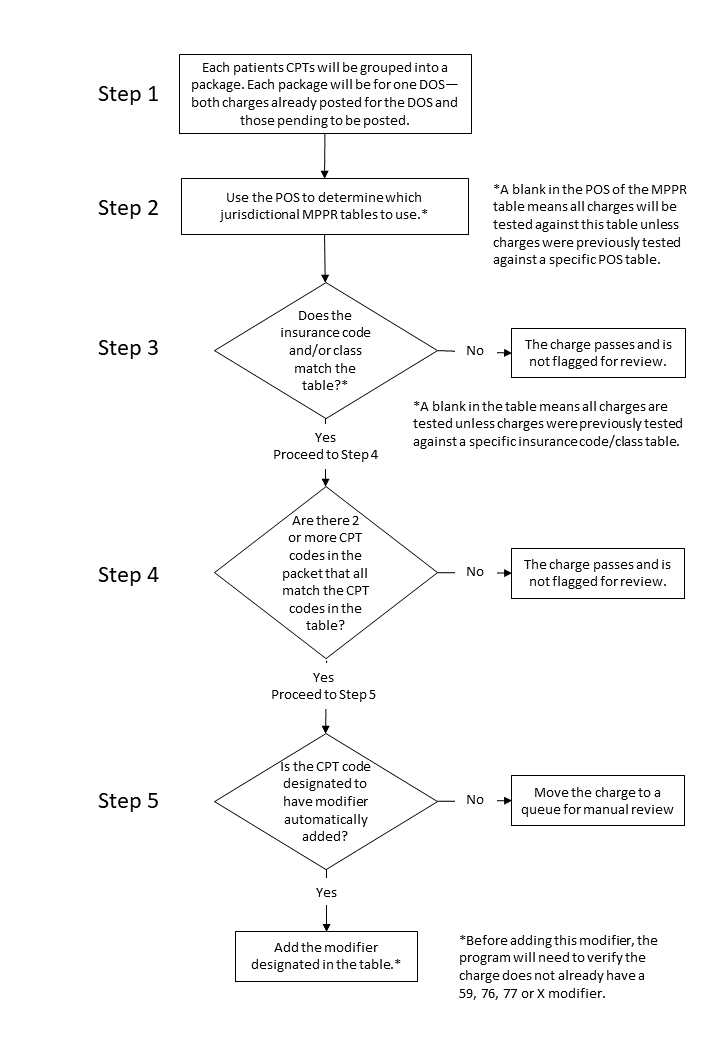
4. Multiple Procedure Payment Reductions (MPPR) Edits CPT Codes
MI will use the following process flow to determine correct modifiers to either automatically add to the charge or send the charge to a queue for further review. A MPPR table will be maintained. This table will have no value in C2 and ony values in C1 will be used for testing.
Notes:
- The multiple procedure payment reduction process (MPPR), is intended to find scenarios where, for example, there are 2 different MRIs or 2 different CTs or an MRI and an US for the same patient and same DOS. If this occurs for a commercial payer we automatically add a 59 modifier. If this occurs for a Medicare payer, the charges are reviewed to determine if different doctors or time span is greater than an hour, and if yes, then add the 59 and if no, then no modifier.
- These CPTs were specifically addressed in our current NCCI processing logic for manual review 36215, 36216, 36217, 36245, 36246, 36247, 36251, 36252, 36253, 36254). They were not specifically NCCI issues but, due to the dollar amounts involved, were set for manual review and can be addressed through a different reporting rule assigned in MI.
- If you have a C1 CPT code that is also a C2 code, this CPT code may get a modifier because it’s a C2 code – this seems appropriate. Notation for CPT codes that appear in both the C1 column and C2 column of NCCI edits.
- Must have a report of all charges wherein the system auto added the modifier.
- Some discussion about each additional CPT codes – seems that since they won’t be on the NCCI tables and we won’t list them on the recurrent tables, this should not be an issue. In other words, these will bill and not be flagged for review.
- Some discussion on CPT codes that include guidance, this will be handled be a separate rule within the MI software.